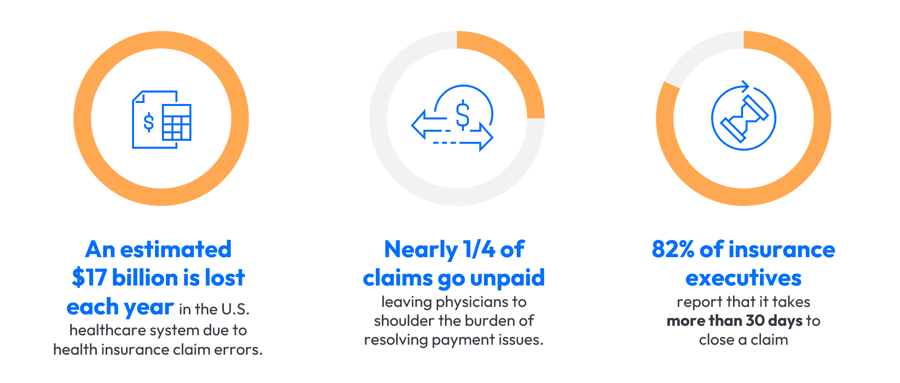
The U.S. healthcare system loses an estimated $17 billion each year due to inefficiencies in claims processing, with nearly one in four claims going unpaid. Additionally, 82% of insurance executives report that it takes more than 30 days to close a single claim.
Delays like this can strain provider cash flow and burden administrative teams with repetitive work.
Against this backdrop, the latest LGI webinar explored how Robotic Process Automation (RPA) is helping healthcare organizations overcome these challenges. Darren Mitchell, Administrator of Business Operations at Medical Associates of Northwest Arkansas (MANA), shared how his team successfully cleared a $1.8 million claims backlog using RPA.
Understanding Robotic Process Automation (RPA): What it is and why it matters.
Before diving into MANA’s experience, it’s important to clarify what RPA is and how it differs from similar technologies like AI.
Robotic Process Automation (RPA) refers to software "robots" that perform routine, rules-based tasks by mimicking human actions. In healthcare, this can include automating claims submissions, processing refunds, verifying insurance, and more. If you can train a person to do it step-by-step, chances are, RPA can do it faster and without fatigue.
Unlike AI, which interprets data and makes probabilistic decisions, RPA works best with structured, repeatable workflows. The kind of workflows that often bog down revenue cycle teams with manual clicking, checking, and keying.
What is MANA’s role in healthcare and who is Darren Mitchell?
MANA is an independent, physician-owned multispecialty group in Northwest Arkansas, offering services in family medicine, pediatric psychiatry, rheumatology, pulmonology, endocrinology, and more. With rapid organizational growth, managing back-end operations became a mounting challenge. As for Darren Mitchell, he brings over 20 years of experience across various healthcare environments, overseeing business operations for the 130 providers and 26 locations of MANA.

Understanding MANA’s challenges with claims processing efficiency.
Darren described a common but critical issue: scaling operations without proportionally increasing staff. Despite solid cash collections, MANA’s refund processing was falling behind. A small three-person team was managing credit balances, with over $1.8 million in unresolved cases and some claims more than four years old.
The bottleneck was unsustainable. They were rolling over $36,000 in unprocessed claims monthly, and the volume was growing.
What MANA Achieved by Implementing RPA
The outcomes were remarkable:
- Pre-RPA: 3 FTEs processed ~400 claims weekly, ~$25–28K/month.
- Testing RPA: $75,000 worth of claims were processed in hours.
- Total Impact: The entire $1.8M backlog cleared with RPA.
- Staff Optimization: 2 FTEs were reassigned to collections, boosting AR outcomes.
In short, what once took months of human effort was now accomplished in hours.

Key factors MANA considered when choosing a solution.
When assessing automation solutions, Darren had four main criteria:
- Ease of management – Minimal day-to-day oversight required.
- Scalability – Could the system handle growth without needing more FTEs?
- Simplicity – Easy to train new staff in case of turnover.
- Partnership – Ongoing support and a collaborative vendor relationship.
LGI’s team met these needs with their tailored RPA approach and industry experience.

Integrating the RPA solution:
Using eClinicalWorks as their EMR, MANA had concerns about the complexity of integrating automation into a multi-click, multi-step process. Darren worked with LGI to break down those barriers. In collaboration with LGI, MANA mapped out a bot-driven workflow: from patient lookup and credit validation to applying refunds based on business rules (e.g., future appointments within 90 days).

Darren’s advice for organizations considering RPA
“Ask the question,” Darren advises. Even complex, click-heavy processes can often be automated. “There’s nothing I’ve shown LGI that they haven’t been able to do.” He emphasizes that processes requiring constant manual intervention—especially those that are repetitive, rules-driven, and must run daily—are prime candidates for automation.
What could automation do for you?
As you reflect on Darren Mitchell’s story, consider this: what routine task is holding your team back right now? Maybe it’s a manual workflow in billing, or a daily admin task that seems too complex to automate. Even if it feels impossible, chances are it’s not.
From revenue cycle management and system data migrations to physician credentialing, patient data collection, payroll updates, and results reporting, we’ve automated some of the most complex, high-volume processes in healthcare.
If a task can be clearly defined and taught to a person, it can likely be automated, allowing digital workers to complement human teams by taking on routine processes and freeing up staff.
Contact the LGI RPA team today to explore what’s possible for your organization.






